Climate change exacerbates the spread of infectious diseases and disrupts vaccine distribution, impacting public health. A rise in environmental conditions favorable to pathogens, alongside increasing vaccine hesitancy driven by misinformation, presents a critical situation that threatens global health efforts. Addressing these intertwined challenges is essential for maintaining effective immunization programs.
Climate change is significantly reshaping global health by altering disease environments and disrupting vaccine distribution, posing a direct threat to public health. The World Health Organization (WHO) estimates that over 154 million lives have been saved due to vaccinations in the past fifty years. However, extreme weather events and global warming are damaging vaccine supplies, complicating their transportation, and potentially decreasing their efficacy. This precarious situation is compounded by rising vaccine hesitancy, particularly following negative societal attitudes fueled by the COVID-19 pandemic and political rhetoric against vaccination.
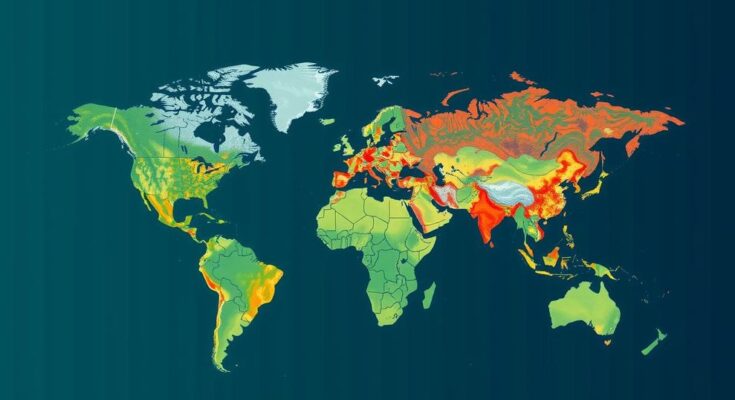
Warmer and wetter climate conditions are fostering environments conducive to the spread of infectious diseases, particularly cholera and dengue fever. These diseases are particularly prevalent in low-income regions, where extreme weather events create ideal conditions for disease outbreaks. The WHO has noted an increase in cholera cases globally since 2021, exacerbated by environmental factors linked to climate change. For instance, floods in Africa have provided supportive habitats for the bacterium Vibrio cholerae, intensifying outbreak severity in vulnerable areas.
Moreover, vaccines that could mitigate the effects of these diseases are also at risk. Research indicates that high temperatures can degrade certain vaccine components, significantly impacting their effectiveness. To combat diseases like cholera and dengue, specific vaccines require careful storage; during extreme weather events, such as hurricanes, disruptions in power can lead to vaccine spoilage. Furthermore, fluctuations in temperature and humidity can directly impact vaccines’ stability and shelf life.
The human response to vaccination is also jeopardized by climate change. Environmental temperature extremes can alter a person’s immune response, leading to adverse reactions or decreased efficacy after vaccination. Thus, as climate conditions worsen, the effectiveness of vaccinations may be compromised, resulting in a further decline in public health resilience.
In addition to these scientific concerns, societal factors are simultaneously undermining vaccination efforts. A noteworthy increase in vaccine misinformation, particularly across social media platforms, has had a considerable impact on public perceptions of vaccines. Political figures and advocacy groups have engaged in campaigns disparaging vaccination, leading to an erosion of public trust in health institutions. Recent statements from prominent political figures have further intensified the dialogue around vaccine hesitancy and misinformation, complicating ongoing public health strategies.
The intertwining challenges of vaccine hesitancy and climate change represent a critical public health concern. Experts advocate for greater transparency and accountability from both political leaders and health organizations to restore public confidence in vaccinations. Effective communication strategies and public education are crucial in combating misinformation and rebuilding trust.
The article discusses the intersection of climate change and vaccination efforts, highlighting how changing climatic conditions are increasing the prevalence of infectious diseases while simultaneously disrupting healthcare initiatives needed to combat those diseases. Specifically, it examines how environmental factors worsen disease spread and affect vaccine efficacy and distribution, ultimately threatening public health strategies that have successfully reduced mortality rates over the decades. The growing hesitancy towards vaccines, influenced by misinformation and political rhetoric, further complicates these public health challenges.
In conclusion, the dual threats of climate change and vaccine hesitancy pose significant challenges for global public health. Addressing these issues necessitates urgent action from health authorities and political leaders to ensure vaccine efficacy and restore public trust in immunization efforts. The interplay between environmental and societal factors must be understood and approached comprehensively to safeguard future public health and mitigate the impacts of climate-related disease outbreaks.
Original Source: www.nationalobserver.com