The mpox outbreak in Uganda is significantly escalating, with 830 recorded cases in 19 states and recent clusters of infections near the DRC border. In the past week, Uganda confirmed 61 new cases and one death, primarily affecting adult men. Additionally, Rwanda reported new Marburg virus cases, totaling 66 confirmed cases with a fatality rate of 23%. Vaccination efforts against both mpox and Marburg are ongoing in the region, with new investigational vaccines being introduced.
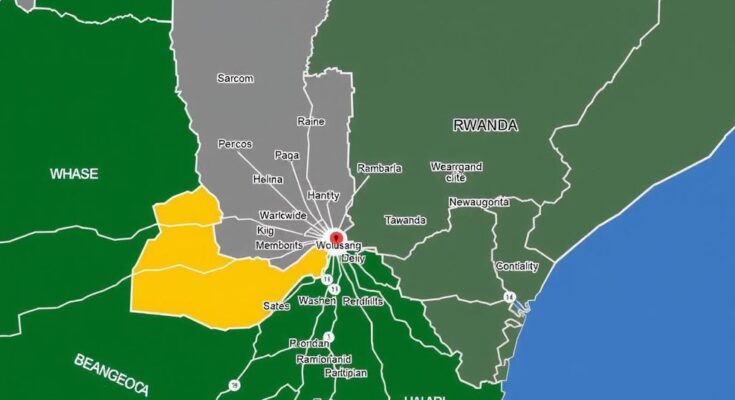
The rise of mpox cases in Uganda has reached alarming levels, with approximately 830 reported cases across 19 states, as highlighted by the Africa Centres for Disease Control and Prevention (Africa CDC). The initial case emerged in the Nakasongola Prison in central Uganda, with subsequent cases mostly concentrated near the border with the Democratic Republic of Congo (DRC) and within fishing communities, prompting health officials to sound the alarm. In the past week alone, health authorities confirmed 61 new mpox cases and a single death. In contrast to the DRC, where children constitute about half of the reported mpox cases, only 12.5% of Uganda’s cases involve children, with a majority (63%) being adult men. The primarily identified strain in Uganda is clade 1b, which is known for its potential sexually transmitted nature. Meanwhile, as mpox cases continue to increase on the continent, Mauritius has reported its first confirmed case and the UK has recorded its initial case of clade 1b stemming from recent travel to an affected region. The African continent has witnessed a total rise of 2,766 mpox cases over the past week, largely concentrated in the DRC and Burundi. So far, nearly 900,000 doses of mpox vaccines have been distributed across nine countries, with vaccination efforts notably progressing in the DRC and Rwanda, while Nigeria has postponed its vaccination initiatives. Simultaneously, Rwanda has reported four additional Marburg virus cases, including a health worker and three contacts of prior cases, raising the total confirmed cases to 66, with a case-fatality rate of approximately 23%. The recent surge includes two deaths within the past week. Investigation into the outbreak has traced it back to fruit bats in a mine near Kigali, which caused infection in the original case. Notably, the Sabin Vaccine Institute has supplied an additional 1,000 investigational Marburg vaccines for ongoing clinical trials in Rwanda. The updated protocol, sponsored by the Rwanda Biomedical Centre, allows for the immediate vaccination of at-risk individuals, including mine workers. This study aims to assess the effectiveness of a single-dose vaccine while ensuring the rapid response to an ongoing Marburg outbreak. As Rwanda continues to navigate the complexities of these health emergencies, coordination and strategic responses remain critical.
Mpox, formerly known as monkeypox, is a zoonotic viral disease that has increasingly affected several African nations, particularly Uganda and the Democratic Republic of Congo. The recent surge in Uganda has raised alarms among health officials due to its significant increase in cases and potential for community transmission. The virus is known to primarily affect adult males in Uganda, differing from trends observed in the DRC where children are more affected. Concurrently, the Marburg virus poses another threat in the region, with Rwanda facing a notable outbreak linked to bats. The response to both mpox and Marburg involves extensive vaccination campaigns to curb their spread, supported by international health organizations and local health ministries.
In conclusion, the burgeoning mpox outbreak in Uganda demands immediate attention and a coordinated healthcare response, particularly given the growing case numbers and their implications for communities. Moreover, Rwanda’s struggle with the Marburg virus underscores the imperatives of timely vaccination and public health measures. The dynamic between these two viral outbreaks, alongside the broader efforts to control infectious diseases within the region, emphasizes the need for enhanced resource allocation, public health awareness, and cross-border collaboration.
Original Source: healthpolicy-watch.news